Article Written by Tim McGonigle, PT
Please forward this to anyone you know who is struggling with low back issues.
Most lumbar problems are preventable and manageable through conservative measures. As with many other health related issues, a critical underemphasized component to successful management is strong personal engagement. Empowering people to effectively influence their health should be the foundation of all medical interventions. Truly mitigating low back problems is possible only when the person is fully engaged in their care as their follow-through and behavior often determines the outcome of others’ interventions. Other-centric interventions (interventions that are centered around others’ responsibilities and actions) should serve as supplemental services to address aspects of a presentation that are beyond the individual’s influence, not as the primary treatment tools. Such a personal-centric system could solve the low back pain crisis (and America’s overall health crisis) that is disrupting so many people’s lives and placing such an economic strain on society.
Low back pain is ubiquitous. It is estimated that 80% of people will seek treatment for lumbar issues at some point during their lives, and many believe the other 20% just don’t take the time to seek help. It has plagued people since the beginning of time and has led to the development of entire industries capitalizing off diagnostic and treatment options. The problem is so great that a panel of experts was assembled to assess the situation worldwide. In 2018, their findings were presented in the renowned British medical journal, The Lancet. It was a three-part report that discussed the scope of the problem, the effectiveness of current interventions and recommendations for the future. It presented a bleak outlook. They reported that the low back problem was becoming so great that it threatened to bankrupt some countries due to the medical cost incurred, lost production and disability payments. Further, they noted that overall diagnostic tests were ineffective in leading to productive interventions and that no treatment was found to be consistently effective in mitigating lumbar pain. Their recommendation was essentially to stop performing diagnostic tests and to minimize the use of treatment modalities so that societies stopped throwing good money after bad! This is not exactly what the person suffering from lumbar pain wants to hear. The panel’s focus was assessing interventions others could provide to those suffering from back pain as these are the interventions that are widely available. If other-centric interventions are ineffective in truly mitigating health issues, such as low back pain, perhaps another avenue should be explored.
As with most musculoskeletal problems, the majority of initial acute lumbar episodes resolve within 1 to 16 weeks. Even most cases with a frank disc herniation creating significant back and leg symptoms start to resolve in 10 to 12 weeks as the disc material is absorbed through the natural healing process. These are often the cases in which epidural injections are helpful in mitigating the person’s suffering while they are waiting for the natural healing process to do its job.
Once structural damage has occurred and the accelerated degenerative process is set into motion due to the wear and tear of life, aging or trauma, musculoskeletal problems never truly fully resolve and management over a lifetime rather than the search for a resolution is the most productive and rational strategy.
It has been clear for decades that surgery is an effective intervention for only about 1% of lumbar patients. These are the ones with an overall healthy lumbar structure except for a single large disc herniation that can be seen encroaching on a nerve root creating a clear pattern of Sciatic nerve irritation that is not resolving with time. With today’s technology a minimally invasive surgical procedure can remove some of the disc material and relieve much of the pressure on the nerve root, significantly reducing the intensity of the pain experienced. However, success is a relative term. Studies show that 25% of those with successful lumbar discectomies still experience some degree of lower extremity pain and that 75% still experience low back pain. These statistics are also true for those who recover from a significant episode that was reduced by natural means.
Some people do have enough instability in a lumbar segment that a fusion is a viable option and when it is necessary, it is necessary. Again, this is the case in a very small percentage of those suffering from low back pain. Studies also indicate that, on average, it takes about eight years for the vertebral levels above or below the fusion to become problematic due to the extra mechanical stress they are subjected to. Again, pointing out that prevention and management over time should become the primary focus.
In reality, it is the persistent lumbar and lower extremity ache with perhaps episodic bouts of more severe pain presentations without clear injection or surgical intervention targets that make up the vast majority of back pain cases. It is these cases that medical science struggles with and that has been the impetus for so much debate regarding the care of the low back pain population. To date, effective intervention has appeared elusive, perhaps because the search has been with the wrong focus.
The search for a scalable, simple algorithm
Due to the magnitude of the low back problem it is reasonable society looks for cost-effective models that can easily be scaled to mitigate its impact. To date, these scalable interventions have been other-centric (Pharmaceutical or medical device/procedure interventions) and largely neglect the importance of the individual’s engaged participation. Without it, coming up with one-size-fits-all, other-centric, and cost-effective intervention(s) that can be easily scaled will remain elusive. This realization leads to the “Doing nothing except letting it run its course” mantra from those holding the purse strings, tying the hands of providers and leaving patients with nowhere to turn.
Mindset
It is human nature to hope for easy, low energy solutions to disruptions in our lives. The search for the one and done intervention for low back problems from clients and providers is a fundamental factor in the failed system. Seeking resolutions to problems so that they no longer require attention is understandable, but with our health it is most often not realistic. Everything in the universe trends towards disorganization/degeneration. Life starts out with a massive proliferation of new cells and growth but in our early 20’s the trend changes to the slow decay of our tissues and systems. A resolution to this slow decay is not possible and the desire for it is a fundamental cornerstone in failed musculoskeletal management. As with other aspects of health, musculoskeletal problems need to be actively managed to mitigate the rate of decay occurring. The transition in mindset from searching for a cure to ongoing active engagement is a primary key to success in the management of low back problems. When one hopes for a resolution (unlimited tolerance without maintenance) it causes them to ignore their ongoing responsibility in the process and tempts them to test the limits to see if a resolution has truly occurred. Frustration emerges as repeated episodes persist, promoting the search for the magic intervention that will finally produce the resolution they seek. While medical and alternative interventions can play a part in managing lumbar pathology, without the client’s ongoing participation poor overall success is inevitable.
The only truly productive strategy for sustained management of lumbar pathology
Accepting that mitigating and managing the inevitable degenerative process is a far more realistic strategy than looking for a resolution sets the stage for productive management. A clear example can be seen in dental care. 100 years ago it was unheard of for someone to get into their 30’s or 40’s and still have all their teeth and healthy gums. Today it is the expected norm for those with access to good care. Why is it so? Because the dental association’s campaign to get people to brush, floss, water-pick, minimize sugary foods and have hygienist visits twice a year has made it possible to preserve oral health over a lifetime. Without the client’s participation and consistent hygienist visits this success would not be possible.
By understanding how to preserve spinal health and facilitating consistent personal compliance, the management of lumbar issues could become as successful as dentists have been in mitigating tooth decay and gum disease.
In spite of the evolving presentation of lumbar pathology with age there are common denominators that lead to successful mitigation strategies over a lifetime. Prevention is always the best medicine. Looking down the road to see where it leads can provide the motivation for buy-in before symptoms occur, but it would take societal support and a wise person to be so proactive. The dentist, of course, had the advantage of the law of natural attraction – “If I have white teeth and fresh breath, she might kiss me!” Convincing a person without back pain to become proactive is more challenging but if doing so became the societal norm many would follow. As with dental care, the same strategy for preventing low back problems can be utilized to mitigate problems once they occur.
The bottom line is this, if stresses exceed the tolerance and remodeling capacity of a tissue or system, breakdown will occur. As breakdown occurs, tolerance and remodeling capacity wane so it takes less stress to cause more trouble. A common pattern can be seen in the deterioration of our lumbar tissues. In our youth (20’s, 30’s, 40’s, 50’s) sitting, standing or working in the garden for a certain length of time produces fatigue of our lumbar structures. As time passes and tissue degeneration occurs it takes less time for more ache to occur with a longer recovery time. If stresses really exceed the tolerance of tissues a flare occurs. If the sprain is not bad and our healing properties are good, the flare resolves. Unfortunately, as time passes, flares become more frequent and require more time to resolve, often with a less-than-full recovery as a vulnerable sensation in the tissues remains. Without a change in strategy, the pattern will repeat, becoming more severe and cumbersome to manage.
By understanding how to mitigate the tissue’s stressors and enhancing one’s remodeling capacity the pattern becomes within the person’s control. There are two mechanical forces (stressors) and if either exceed the tolerance and remodeling capacity of one’s lumbar tissues breakdown will occur. These are (1) Positions that take all the slack out of tissues creating a sharp increase in either tensile or compression stresses, and (2) Axial loading creating a compressive stress on tissues. Once understood, easy strategies can be introduced to mitigate these stresses during activities of daily living (ADL’s) and exercise training, thereby keeping the accumulation of stressors within the tolerance and remodeling capacity of lumbar tissues so they remain asymptomatic over a lifetime.
For example, mitigating axial loading can be achieved:
- With the use of shock absorbing surfaces (shoes, shoe inserts, kitchen/workplace mats, etc.) and the use of elastic lumbar corsets.
- By breaking up weight bearing activities with getting non-weight bearing (lying down), getting in a supported reclining position of at least 45˚, or applying self-traction to the lumbar region before structural fatigue occurs.
- Performing exercises that involve pushing or pulling down instead of pulling or pushing up activities or simply performing exercises in horizontal instead of vertical positions.
- Using hiking poles when the activity involves prolonged standing or walking. Or utilizing crutches or a walker if the lumbar tissue’s tolerance for axial loading is very poor.
Controlling position forces involves mitigating end-of-range stresses from accumulating using ergonomics, muscular control, respecting limits of movement during ADL’s (activities of daily living) and exercise. As this requires coaching, body awareness, strength, endurance and coordination becoming proficient at this aspect of back care usually requires some guided individual training, as is the case with learning all life and motor skills.
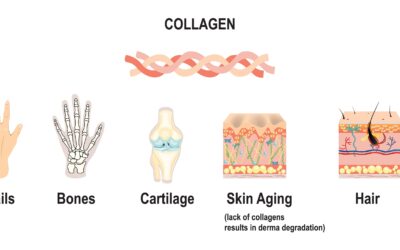
Optimizing tissue health and remodeling capacity requires good overall lifestyle habits including not smoking, controlling stress, getting adequate sleep, eating well, consistent exercise, and getting periodic bodywork/massage to keep connective tissue supple.
It has been said that the three keys to health are circulation, circulation and circulation. There is evidence that disc degeneration correlates with high cholesterol levels as the small vessels that travel from the aorta to the vertebral bodies and outer rim of the disc can become blocked, reducing blood supply and accelerating the deterioration of these tissues. Optimal circulation is dependent on cardiovascular fitness, body movement and muscular action to push fluids along, combined with open arteries and pliable connective tissues to minimize resistance to flow. Static positions (Prolonged sitting, standing or lying) have been described as the “New smoking” as they inhibit circulation and lead to tissue decay. The compression produced by prolonged axial loading of sitting and standing further inhibits circulation from occurring in the discs, vertebral bodies and spinal canal. Spinal structures are particularly vulnerable to poor circulation from clogged arteries, or the lack of movement and pressure changes due to the small diameter of the vessels. Additionally, the inner disc tissues do not have a direct blood supply and are dependent on movement and changes in pressure to facilitate diffusion of nutrients from the blood-rich vertebral bodies.
Muscular support is critical to the health and longevity of lumbar tissues as without active support from the surrounding muscles it is nearly impossible to control position forces during activity. Good muscle mass also provides some passive support to the vertebral structures even when the muscles are fairly relaxed. Additionally, much of the discomfort associated with back and leg pain can stem from the surrounding muscles and soft tissues, just as someone can have pain from a Rotator Cuff problem or patellar tendonitis. Knee and shoulder pain are often alleviated by addressing soft tissue findings and restoring more optimal muscle control and muscle mass. The same is true with back and leg pain. With proper instructions, optimal motor function can be safely restored if axial loading and position forces are controlled. A well-thought-out exercise program can stimulate a positive cascade of events that mitigate back pain by enhancing circulation, body sense, strength, endurance, coordination, becoming aware of physical limits, restoring confidence/reducing fear of movement, desensitizing the nervous system, etc. As intensity matters, guided instructions and supervision are often necessary until the participant is confident in their ability to utilize proper technique throughout the duration of the program.
Mitigating position forces dissipating through lumbar tissues is also achieved by restoring more optimal mobility of a person’s thoracic cage, hips and lower extremity muscles. As forces follow the path of least resistance, if these structures are tight forces have no other choice but to dissipate through the more vulnerable lumbar structures. If these stresses exceed tissue tolerance and remodeling capacity, over challenging will occur precipitating or perpetuating one’s low back pain.
Of primary importance in the prevention and management of lumbar problems is the willingness of the individual to be proactive. The common patterns responsible for failed intervention are the tendencies for people to either stop engaging with normal life activities, or to ignore the early signs of structural fatigue during activity and persisting into symptoms until their magnitude forces some level of compliance. No matter how good an intervention has been, if the client does not stay engaged with life or ignores the early signs that structures are being over challenged until real irritation develops, their back problems will persist. No one on the face of the earth has control over these patterns except the person themselves, leaving the success or failure of intervention at the mercy of the individual’s behavior.
By changing the search for a resolution to one of proactive management and giving people the understanding that they must stay active while preventing position and compressive forces from over challenging tissues, sustained success is achievable. Without this change in mindset, success will remain elusive as the individual will either unwittingly succumb to the pearls of inactivity and social isolation or perpetuate the overchallenging of their tissues resulting in ongoing symptoms. Without activity, all tissues and body systems weaken, circulation slows, and backs will ache. Unless a sudden trauma occurs, such as a fall, our tissues usually send out warnings of being either under or over challenged. It begins with a sense of fatigue, which if ignored turns into ache, which if ignored turns into pain, which if ignored turns into a significant flare.
The key is to stay active and engaged in life while mitigating axial loading and position forces to optimize functional tolerance, to accept one’s limits and to prevent the tissue over challenging cascade by taking breaks or performing some self-care before fatigue sets in during activity. By doing so, fatigue will not lead to ache, which never develops into pain and flares are prevented. The old saying, “A stitch in time saves nine” is absolutely true.
The Good News
With understanding and the appropriate tools, prevention and management of low back issues are largely within one’s control. It does require active and consistent participation from the individual. Facilitating this mindset and personal engagement have been the missing link in the search for mitigating this ubiquitous personal, medical and social problem. And the side effects from full participation – better overall physical, emotional and social health, fitness and mobility. Not bad for a medical intervention!
Most of us require support to stay on track with health promoting habits. I am sure many reading this know they do a better job caring for their teeth in the few weeks before their hygienist appointment. It is human nature to sluff off when no one is watching and to be more on when monitored. Get educated and find the support you need to stay on track over your lifetime. If you live outside of the Folsom Area, please feel free to call to see if we have trained someone in your area who will have the skills to assess and address your comprehensive presentation and who may have a cost-effective group exercise program to help keep you on track with productive management of your lumbar issues over your lifetime.